What is achalasia?
Achalasia is an uncommon disorder that causes difficulty with swallowing. Although the condition cannot be cured, the symptoms can usually be controlled with treatment.
What causes achalasia?
The main cause of achalasia is degeneration of the nerve cells in the esophagus (the food pipe). The exact reason why this happens is not known. The loss of nerve cells in the esophagus causes two major problems that interfere with swallowing. Firstly, the muscles that line the esophagus do not contract normally, so that swallowed food is not pushed forward through the esophagus and into the stomach properly. Secondly, the lower esophageal sphincter (LES), a valve made of of muscles does not relaxe normally with swallowing as it does in normal people. As a result of this the esophagus above the persistently contracted LES starts to dilate, and large volumes of food and saliva can accumulate in the dilated esophagus.
Mechanism of achalasia
What symptoms do patients with achalasia experience?
The commonest symptom of achalasia is difficulty in swallowing. Patients get a sensation that swallowed food as well as liquids get stuck in the chest. This problem invariably progresses and becomes severe. Other symptoms include regurgitation of swallowed food and liquid, chest pain, heartburn, a sensation of fullness or a lump in the throat, hiccoughs, and weight loss.
How is achalasia diagnosed?
The doctors can suspect achalasia based on the symptoms and order certain tests to confirm the diagnosis.
1. Barium swallow: The barium swallow involves swallowing a milky liquid of barium while x-rays are taken. In patients with achalasia the barium swallow shows a narrow region at the lower end of the esophagus (bird’s beak) with a dilated esophagus above this
Barium swallow shows narroowing
at lower end of esophagus (arrow)
2. Endoscopy: In this test the doctor passes a thin, lighted, flexible tube via the mouth to see the inside of the esophagus, LES, and stomach. Most patients are given an intravenous sedative during the endoscopy procedure to make them sleepy and relaxed.
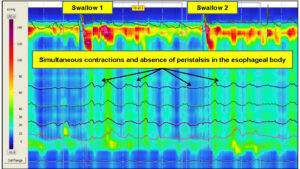
3. Manometry: Manometry involves the passage of a thin tube through the mouth or nose into the esophagus. The tube is lined by numerous pressure sensors that convey pressures within the esophagus to a device. The test measures the changes in pressures within the esophagus that are caused by the contraction of the muscles esophagus. Manometry is almost always used to confirm the diagnosis of achalasia. The test typically reveals three abnormalities in people with achalasia: high pressure in the LES at rest, failure of the LES to relax after swallowing, and an absence of useful (peristaltic) contractions in the lower esophagus.
Manometry report in achalasia
How is achalasia treated?
The many options available for treating patients with achalasia cannot stop or reverse the underlying loss of nerve cells in the esophagus or restore the normal peristaltic cntractions in the esophagus. Rather, the treatments aim to weaken the lower esophageal sphincter (LES) muscle to the point that it no longer acts as a barrier to the passage of food and liquids.
1. Drugs: Two types of drugs, nitrates and calcium channel blockers, may be used for relaxing the LES muscle. However, in the long term the drug therapy is inconvenient, ineffective, and often associated with unpleasant side effects, such as headache and low blood pressure. Also, the drugs tend to become less effective over time.
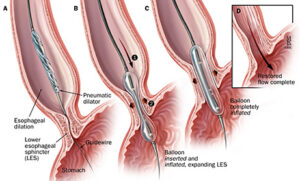
2. Balloon dilatation: This procedure is carried out under sedation. After preliminary endoscopy, a collapsed balloon is passed through the mouth and positioned in the region of the LES using guidance from an x-ray machine. It is then inflated in order to tear the muscle of the LES. The effect of a balloon dilatation in relieving the symptoms is temporary; most patients require multiple balloon dilatations at progressively shorter intervals and eventually require surgery. The most serious complication of a balloon dilatation is perforation (creation of a hole) of the esophagus, which occurs in 1% – 6% patients. The risk of a perforation increases with repeated dilatations. Because the LES has been made ineffective, 2% – 5% patients also develop gastroesophageal reflux disease (GERD) after balloon dilation. Also, after repeated dilatations the surgery, when it is eventually required, becomes more chalenging. For these reasons, this treatment is best reserved for patients who are unfit for surgery due to old age or medical conditions which make administration of general anesthetic risky. Young and fit patients not wishing to undergo surgery upon diagnosis of achalasia may be offered one dilatation, but are best councelled regarding surgery when the symptoms recur.
Balloon dilatation in achalasia
3. Botulinum toxin injection: Injection of botulinum toxin (botox) into the LES under endoscopic guidance temporarily paralyzes the nerves that make the LES contract, thereby helping to relieve the obstruction. The relief of sympotms with this expensive therapy is short term (3 – 12 months). Also, repeated injections create scarring in the muscles of the LES, and make the subsequent surgery more challenging. This treatment, once quite popular, has fallen out of vogue recently.
How can surgery help patients with achalasia?
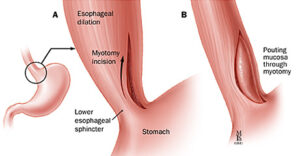
The surgery performed to treat patients with achalasia is called cardiomyotomy (division of the muscles of the LES and upper end of stomach). In the past this surgery was performed through a large open incision in the upper abdomen. Today, it is carried out laparoscopically.
How is a laparosocpic cardiomyotomy performed?
This operation is performed under general anaesthesia. The surgeon makes a small (1cm) in the upper abdomen and introduces a cannula or a tube inside the abdomen. He will insert a telescope attached to a miniature video camera through the cannula that gives him and the operating team a magnified view of your internal organs on a video monitor. He will then place four other additional cannulas through tiny (5mm) cuts to accommodate special long instruments. At the surgery, the LES and the muscle layer in the upper part of the stomach are divided precisely under the magnified view. As division of LES makes the patient prone to GERD, a part of the stomach called fundus is rotated around and fixed in such a way that it creates a fundoplication or a weak valve. This prevents the acid from the stomach from coming back into the esophagus.
Laparoscopic myotomy removes the blockage
What happens after a laparoscopic cardiomyotomy?
The patient does experience some amount of pain for about 12 to 24 hours after laparoscopic fundoplication depending on individual tolerance. Also, some nausea and vomiting is not uncommon in the first 12 hours. Patients are always given medications to relieve the pain and take care of the nausea. Usually, the patient is allowed to drink fluids within 6 to 8 hours of surgery and is allowed soft blenderized food from the day after surgery. Activity is dependent on how the patient feels, but all patients are encouraged to get up and walk as soon as they are comfortable. Most patients go home within a 48 – 72 hours after laparoscopic cardiomyotomy In general, patients recover completely within 10 – 15 days. All patients having a cardiomyotomy need to follow a blenderized diet for around 6 weeks as the area of surgery is healing. Also they are advised to avoid eat slowly, eat small frequent meals and avoid carbonated drinks. After the initial period of 6 weeks a patient is allowed to eat normal food.
How soon can I resume work?
In our society patients often prefer to take things easy for weeks after any operation because of a fear that they may harm themselves by being active. After laparoscopic cholecystectomy the recovery is quite rapid. Soon after returning home the patients are allowed all activities they feel comfortable with. Depending on the nature of their job, most patients are able to return to work within ten to fifteen days following a laparoscopic cardiomyotomy. Patients with light, desk jobs usually return in a few days while those involved in heavy lifting may require a little more time.
What are the advantages of laparoscopic cardiomyotomy?
Less pain from the incisions after surgery
Shorter hospital stay
Shorter recovery time
Faster return to normal diet
Faster return to work or normal activity
Better cosmetic healing
What follow up is required after surgery?
Since none of the treatments for achalasia cure the underlying disease, regular follow-up is essential. People with achalasia have an increased risk of developing esophageal cancer and after surgery there is a small chance of developing gastroesophageal reflux (GERD). The follow up is aimed at recognising and treating recurrent symptoms or complications of treatment (eg, GERD) early.
Dr Deepraj Bhandarkar’s Presentations Related to Surgery for Achalasia
Presentations, invited lectures & videos
Bhandarkar DS, Shah RS. Laparoscopic cardiomyotomy for achalasia cardia. 4th Annual Conference of IAGES, Chennai, 2000.
Bhandarkar DS, Shah RS. Laparoscopic Heller-Dor procedure for achalasia. Annual Conference of Maharashtra Chapter of ASI, Karad, 2000.
Bhandarkar DS. Heller’s cardiomyotomy for achalasia cardia – how I do it. Annual Conference of IASG, Bhopal, 2003.
Katara AN, Bhandarkar DS, Shah RS. Laparoscopic cardiomyotomy for achalasia cardia. Annual Conference of Maharashtra Chapter of ASI, Thane, 2004.
Bhandarkar DS. Laparoscopic surgery for achalasia cardia. 53rd National Conference of International College of Surgeons, Agra, 2007.
Bhandarkar DS. Laparoscopic surgery for achalasia cardia. ICS National Surgical Update, Pune, 2007.
Katara AN, Bhandarkar DS, Shankar M, Kochar R, Udwadia TE. Laparoscopic Heller’s procedure for stage IV achalasia cardia. ELSA 2007, Hyderabad, 2007.
Bhandarkar DS, Katara AN, Kochar R, Udwadia TE. Laparoscopic cardiomyotomy for sigmoid esophagus. MASICON 2008, Kolhapur, 2008.
Bhandarkar DS. Laparoscopic Heller’s myotomy. PSG Surgicon, Coimbatore, 2008.
Bhandarkar DS. Achalasia cardia: balloon, botox or buttonhole surgery? 54th Annual Conference of International College of Surgeons. Trichy, 2008.
Bhandarkar DS. Laparoscopic surgery for achalasia cardia. ASICON 2010, New Delhi, 2010.
Bhandarkar DS. Laparoscopic surgery for achalasia, GERD and paraesophageal hernia. 41st FIAGES course, Gokak, 2015.
Bhandarkar DS. Laparoscopic cardiomyotomy versus POEM for achalasia cardia – a debate. MASICON 2015, Nagpur, 2015.
Bhandarkar DS. Surgery is better than endotherapy for managing achalasia. Debate in Converge 2015. Delhi, 2015.
Bhandarkar DS. Surgical management of achalasia cardia. OG junction CME, Pune 2018.
Bhandarkar DS. Treatment of achalasia cardia – optimising the outcomes. Annual conference of SELSB. E meeting. 2022.